THE FOOT AND ANKLE
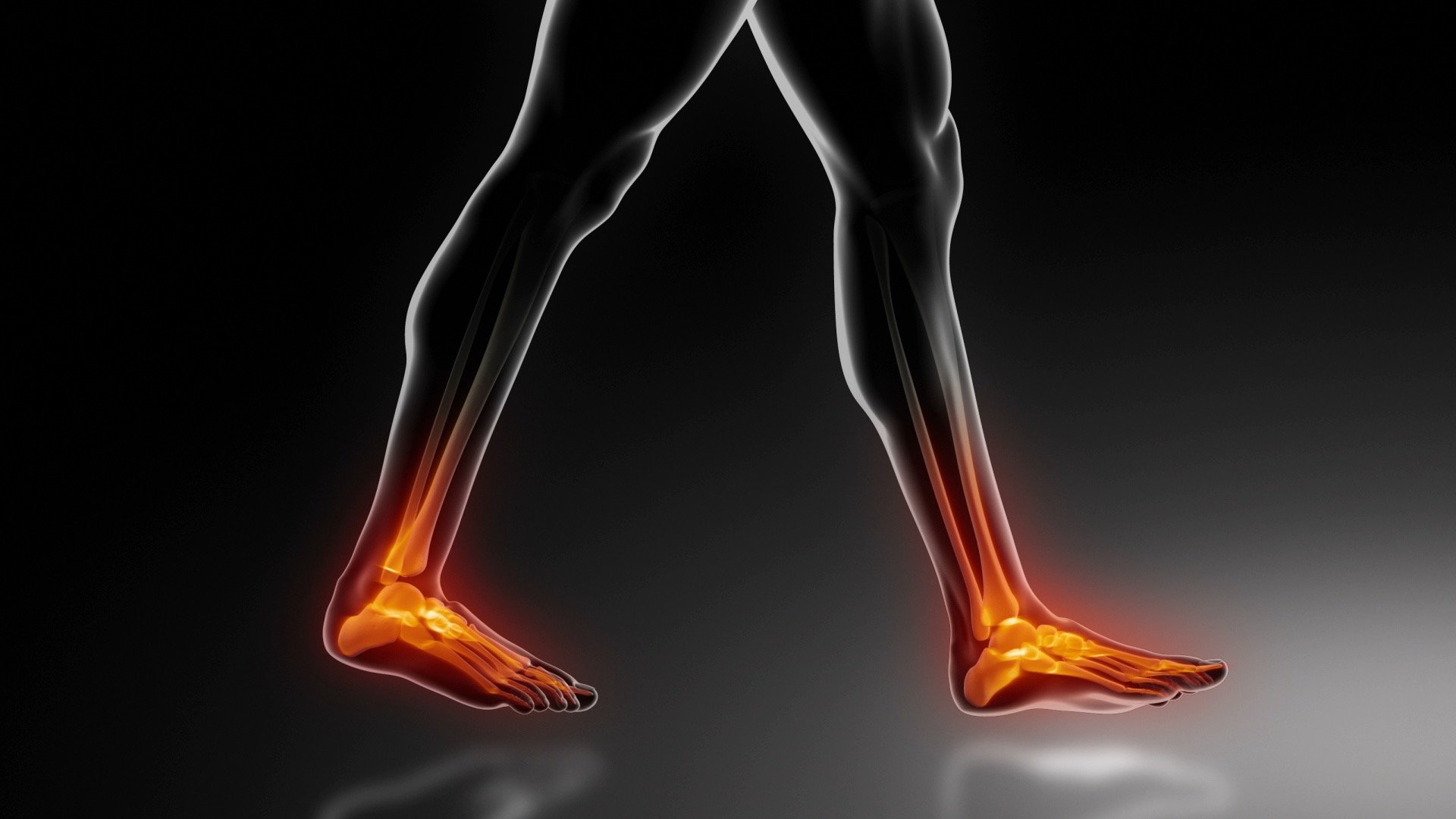
The foot and ankle are complex structures composed of numerous bones, ligaments, tendons, and muscles that work together to provide stability, balance, and movement. The ankle joint connects the foot to the leg, allowing for a wide range of motion, including flexion, extension, inversion, and eversion. The foot, consisting of 26 bones, plays a crucial role in weight-bearing and shock absorption during walking, running, and other activities. The intricate mechanics of the foot and ankle allow for adaptability on various surfaces, but they are also vulnerable to injuries, deformities, and degenerative conditions due to their constant use.
Common foot and ankle problems include sprains, fractures, tendon injuries, arthritis, and conditions like plantar fasciitis and bunions. These issues can cause pain, limited mobility, and difficulty in performing daily activities. Orthopedic surgeons specializing in foot and ankle care provide a range of treatments,
from conservative methods like physical therapy, orthotics, and medications to more advanced surgical procedures. Surgeries such as ankle arthroscopy, tendon repair, and joint fusion are often necessary to address severe injuries or chronic conditions that do not respond to non-surgical treatments. The goal of orthopedic intervention is to relieve pain, restore function, and improve the patient’s quality of life, enabling them to return to their daily activities with greater mobility and confidence.
Some of the most common Foot and Ankle conditions include:
Ankle Sprains
Plantar Fasciitis
Achilles Tendonitis
Ankle Fractures
Bunions (Hallux Valgus)
Hammertoe
Flat Feet (Pes Planus)
Morton’s Neuroma
Tarsal Tunnel Syndrome
Osteoarthritis of the Foot and Ankle
COMMON CONDITIONS
Plantar Fasciitis
Plantar fasciitis is one of the most prevalent causes of heel pain, resulting from inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. The condition often manifests as sharp pain in the heel, especially during the first steps in the morning or after prolonged periods of sitting or standing. Risk factors include obesity, prolonged standing, improper footwear, and certain physical activities, such as running or dancing. For many patients, the pain can be debilitating, significantly affecting their daily activities and quality of life.
Orthopedic treatment for plantar fasciitis typically begins with conservative measures, such as rest, ice therapy, stretching exercises, and the use of orthotic inserts to provide arch support. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to alleviate pain and reduce inflammation. If conservative treatments fail to provide relief after several months, more advanced interventions may be considered, including corticosteroid injections, physical therapy, or, in severe cases, surgery to release the plantar fascia. With appropriate treatment, most patients can expect significant improvement in their symptoms and a return to normal activities.
Achilles Tendonitis
Achilles tendonitis is an overuse injury characterized by inflammation of the Achilles tendon, which connects the calf muscles to the heel bone. It commonly affects runners, dancers, and individuals who engage in sports that involve repetitive stress on the tendon. Patients typically experience pain and stiffness along the tendon, particularly near the heel, which may worsen with activity or after prolonged periods of inactivity. If left untreated, the condition can lead to more severe issues, including tendon rupture, which requires surgical intervention.
Treatment for Achilles tendonitis often begins with conservative measures, including rest, ice, and the use of anti-inflammatory medications to reduce pain and swelling. Physical therapy may be recommended to strengthen the calf muscles and improve flexibility in the tendon. Patients are also advised to modify their activities and wear supportive footwear. If symptoms persist despite conservative treatment, orthopedic surgeons may consider more invasive options, such as corticosteroid injections or surgery to repair any damage to the tendon. Most patients respond well to treatment and can return to their normal activities with proper care and rehabilitation.
COMMON PROCEDURES
Ankle Arthroscopy
Ankle arthroscopy is a minimally invasive surgical procedure used to diagnose and treat various conditions affecting the ankle joint, including ligament injuries, cartilage damage, and impingement syndromes. During the procedure, the orthopedic surgeon inserts a small camera (arthroscope) and specialized instruments through tiny incisions around the ankle. This allows the surgeon to visualize the inside of the joint and perform necessary repairs or debridement without the need for larger incisions. Ankle arthroscopy is often preferred for its reduced recovery time, lower risk of complications, and less postoperative pain compared to traditional open surgery.
Recovery from ankle arthroscopy typically involves a short hospital stay, followed by a period of rehabilitation to restore strength and mobility. Patients are usually encouraged to begin physical therapy shortly after surgery to promote healing and regain function. The minimally invasive nature of the procedure allows many patients to return to normal activities within weeks, depending on the extent of the surgery. Ankle arthroscopy has proven to be an effective treatment option for many ankle conditions, helping patients resume their active lifestyles with improved mobility and reduced pain.
Bunion Surgery (Hallux Valgus Repair)
Bunion surgery, or hallux valgus repair, is performed to correct a bunion deformity, which involves a bony bump that forms at the base of the big toe due to misalignment of the toe joint. This condition can cause pain, inflammation, and difficulty wearing shoes, significantly impacting a patient's quality of life. During the procedure, the orthopedic surgeon realigns the bones of the big toe and removes the bony prominence to restore proper foot function. Various surgical techniques may be employed, including osteotomy (cutting and repositioning bones), and in some cases, the placement of screws or plates to stabilize the joint.
Recovery from bunion surgery can take several weeks to months, depending on the specific procedure and the patient's overall health. Initially, patients may need to wear a specialized postoperative shoe or boot to protect the foot and facilitate healing. Physical therapy may also be recommended to improve range of motion and strengthen the foot. While bunion surgery can provide significant relief from pain and discomfort, patients must adhere to their orthopedic surgeon's post-operative care instructions to ensure optimal healing and a successful return to normal activities. Most patients report improved foot function and comfort after the surgery, allowing them to wear regular footwear without pain.
